Zovirax dosages: 800 mg, 400 mg, 200 mg
Zovirax packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Cheap 400 mg zovirax fast delivery
Injuries that contain concomitant skeletal injuries add an extra level of complexity to the administration of these already challenging vascular injuries. Temporary reperfusion can be accomplished quickly with intraluminal Argyle shunts. The institution of early amputation stays a difficult choice and requires cautious judgment. Even with successful limb salvage, the practical end result could additionally be unsatisfactory secondary to associated nerve harm and significant muscle and osseous tissue loss inclusive of complete compartments. Scores from 7 to 10 have been used to select sufferers who will probably require main amputation. Ultimately the decision to amputate have to be thought of on an individual basis, maintaining in thoughts the best pursuits of the patient. The determination to amputate should involve the whole multidisciplinary group and, if possible, the patient. These issues embody narrowed vessels, intimal flaps, small pseudoaneurysms, and arteriovenous fistulas. However, Frykberg reported that these clinically occult accidents have a mostly benign natural historical past and could be safely observed. In the event that these lesions do deteriorate to the point that they require restore, it can be done without any adverse sequelae. However, this series has a small variety of patients and not a very lengthy follow-up. The senior writer of this chapter considers the popliteal artery to be an finish artery given its small branches and low move characteristic of such branches. Furthermore, the tibial vessels as properly as peroneal artery are prone to significant spasm, which ends up in extended ischemia. Therefore, he recommends that all popliteal arteries must be definitively repaired (Table 4). Acute thrombosis is of scientific importance and, if recognized promptly, can probably be reversed. Technical errors should be suspected within the early postoperative interval and have to be addressed surgically on an immediate foundation. D�bridement of devitalized tissue and removing of any foreign material is crucial during initial or subsequent surgeries. Tissue necrosis and adjoining wound infections can lead to deadly hemorrhage secondary to disruption of the vascular repair. Unfortunately, soft tissue protection may be restricted and additional surgical flaps could also be needed for defense of the vascular repair. Successful limb salvage and long-term follow-up demonstrate the disability associated with popliteal vessel accidents. At the time of discharge, patients having undergone orthopedic restore could require extensive rehabilitation or have the need for mechanical units when ambulating. Nonunion of fractures, knee instability, and osteomyelitis are also well-known orthopedic complications prevalent in the setting of trauma. Neurologic deficits, similar to foot drop secondary to associated perineal nerve damage, either main or as a outcome of an untreated compartment syndrome, do demand the location of a brace as properly as aggressive bodily therapy. Previous limb salvage methods during early wartime proved to be debilitating with excessive incidence of amputation rates in popliteal vessel injuries. Far higher outcomes and decrease amputation rates are appreciated in varied retrospective reviews over the past several a long time. Civilian amputation rates reported in several series are reported to range from 6% to 37%. Extremity compartmental hypertension and limb salvage is a crucial concern at time of injury, presentation, and hospitalization. Continued controversy remains concerning the timing of fasciotomies; however, in the setting of compartment syndrome, quick four-compartment fasciotomy is mandated. The risk of limb loss as a consequence of not promptly performing fasciotomies is stressed in several published reviews.
Discount 200 mg zovirax
In the study by Cicala and colleagues, two sufferers with gunshot wounds to the cervicothoracic trachea developed tension pneumothorax with large air leak during resuscitation. Hemoptysis, along with different findings, was noted in two of the gunshot wound victims. Blunt trauma patients who survive to the emergency division might current with a wide spectrum of scientific signs and symptoms dependant on the severity and location of the injury to the cervical thoracic trachea. Blunt cervical tracheal damage might create extreme respiratory compromise resulting in rapid acute respiratory failure and asphyxia. Alternatively, patients with less extreme injuries could present with stridor, hoarseness, hemoptysis, and subcutaneous emphysema. Indications for bronchoscopy embody a big pneumomediastinum, persistent pneumothorax, or a large, persistent air leak after placement of a functional thoracostomy tube; persistent atelectasis; and increasing severe subcutaneous emphysema. Bronchoscopy is essentially the most accurate and dependable means to set up the diagnosis, decide the location, and outline the extent of the harm. Debate stays as to whether rigid or flexible bronchoscopy is superior in this setting. Disadvantages of rigid bronchoscopy embrace the necessity for a common anesthetic and a stable cervical spine. Preoperative evaluation of the vocal cords on this setting is strongly recommended. The presence of a recurrent laryngeal nerve injury causing vocal wire paralysis might help the operating surgeon in figuring out whether tracheostomy is needed regardless of the location or extent of airway injury. Patients intubated previous to arrival in the emergency division should bear flexible bronchoscopy as soon as possible. Careful intubation over a bronchoscope, carried out by an skilled bronchoscopist, is the optimal approach for these patients who require early airway control for clinical deterioration or for remedy of different life-threatening accidents. Intubation is ideally carried out within the operating room where emergent cricothyroidotomy or tracheostomy could be performed if needed. The trauma surgeon should be ready to prolong the tracheostomy incision to a median sternotomy if the distal trachea retracts into the mediastinum. Clinical deterioration should happen as positive-pressure ventilation is utilized if the injury is distal to the tracheostomy. High-frequency ventilation or low tidal volume ventilation with further tube thoracostomies could also be necessary. Nonoperative Management Small iatrogenic accidents from endotracheal intubation or from minimal blunt trauma can usually be safely noticed. Gomez-Caro et al reported the profitable administration of 17 sufferers with iatrogenic tracheobronchial injuries between 1993 and 2003. The authors reported no problems or deaths instantly caused by nonoperative administration. Guidelines for nonoperative administration embody very important indicators stability, no related esophageal harm, no issues with mechanical ventilation or intubation (if necessary), no improvement of severe subcutaneous emphysema or mediastinal emphysema, and no indicators of sepsis. Additional requirements for nonoperative administration have been printed and embody only small tracheobronchial lacerations, corresponding to those with less than one third of the circumference of the trachea, well-opposed edges, no vital tissue loss, no related accidents, and no want for positivepressure ventilation. When essential, endotracheal intubation with placement of the endotracheal tube balloon distal to the tear has been proposed by Marquette et al. This technique has been successfully used on three occasions by one of the authors. Nonoperative administration consists of administering prophylactic antibiotics and proton pump inhibitors, very close remark, and shut bronchoscopic follow-up. Nonoperative Case Presentation n the patient is a 43-year-old woman who was injured in a high- speed motor vehicle collision. Operative Management Patients diagnosed with a major tracheobronchial damage ought to all the time undergo surgery unless medical instability or extreme related injuries are significantly prohibitive. In those situations, all efforts are made to assist and stabilize the patient while sustaining sufficient oxygenation and ventilation.
Diseases
- Microgastria limb reduction defect
- Gemignani syndrome
- Strongyloidiasis
- Sexually transmitted disease
- Dextrocardia-bronchiectasis-sinusitis
- Nephrocalcinosis
- IgA deficiency
- Phocomelia ectrodactyly deafness sinus arrhythmia
- Renal tubular acidosis
Order zovirax uk
It crosses the nasal septum and posteriorly crosses the posterior maxillary wall and the pterygoid plates. This kind of fracture pattern happens in roughly 30% of all Le Fort fractures. It is normally the result of direct anterior-posterior impacts low on the midface, producing fractures of the vertical and horizontal buttresses of the midface. This fracture often begins on the nasal bones and crosses the frontal strategy of the maxilla and lacrimal bones. It then descends through the ground of the orbit, infraorbital rim, and lateral maxillary sinus wall, extending posteriorly via the pterygoid plates. The ensuing fracture creates a pyramidal fracture of the inferior facial section, which is separated from the remaining craniofacial skeleton. Similarly, as seen in Le Fort I fractures, the fracture traverses the nasal septum, posterior maxillary partitions, and pterygoid plates. This fracture sample is the most common sample of fracture, occurring in nearly 60% of all instances. Such a fracture pattern is usually attributable to oblique forces to the vertical buttress and is the most uncommon of all three fracture patterns. It is often seen in high-velocity impact and associated with important comminution and intracranial harm. Often they demonstrate characteristics of a quantity of Le Fort accidents on opposing sides of the bony facial skeleton. Of all facial fractures, Le Fort fractures are seen in roughly 10% to 20% of sufferers. This pattern of facial fracture is most commonly seen after motorcar accident, interpersonal violence, or falls from height. They usually have a proportionately bigger mandible and frontal bone, combined with extra flexible facial bones, undeveloped maxillary sinuses, and dentition that has not but erupted, all of which stop children from such fracture patterns. Le Fort fractures are often associated with other forms of head and neck injuries, including intracranial, ophthalmologic, and neck accidents. Often bleeding is secondary to mucosal tear of the septal, nasal, or sinus mucosa. Once secure, premorbid dental occlusion and previous historical past of dental trauma are important to verify. A detailed ophthalmologic historical past is also important to analysis for any acute modifications in vision. Examination should also include inspection and palpation of the whole facial skeleton, evaluating for mobility of facial buildings. Malocclusion is usually seen during which a displaced maxilla may result in premature contact or an open bite deformity. Often forces of midface trauma trigger a posterior displacement of the maxilla alongside the cranium base. If the damage has prolonged to the bony orbit, ecchymosis or an irregular globe position could also be encountered. This may be evaluated through the use of the thumb and forefinger to grasp the premaxilla whereas the other hand stabilizes the infraorbital rims. Special consideration ought to be made on imaging via the orbits and the bottom of skull, as intracranial damage could alter the surgical algorithm. Surgical administration of Le Fort fractures is focused on restoration of operate as well as aesthetic aspects of facial symmetry. Reestablishment of facial top and facial projection and reconstitution of premorbid dental occlusion are the primary objectives of surgical repair. It was previously believed that repair of Le Fort fractures ought to await resolution of soft tissue edema, allowing a better analysis of surgical landmarks and a greater postoperative discount. Some authors report earlier return to perform, decreased an infection fee, decreased scarring, and fewer postoperative complications with a direct repair. Midfacial bones could be uncovered by the use of concealed surgical incision by way of a combination of intraoral, transconjunctival, bicoronal, or midface degloving in order to reduce the entire fractured buttresses.
Order zovirax with american express
Interventions to restore renal perfusion, via either open operative or endovascular approaches, have been associated with poor outcomes together with repair failure, want for nephrectomy, infection, renovascular hypertension, and demise. A multicenter research from the Western Trauma Association confirmed the poor outcomes with attempts at vascular repair and demonstrated superior outcomes with either quick or delayed nephrectomy. Most patients ought to both be observed nonoperatively or be thought of for delayed nephrectomy after preliminary evaluation and management of extra urgent injuries. Attempts at revascularization should normally be reserved only for these patients with an early analysis (within 2�4 hours) and with already borderline renal perform, bilateral accidents, or solitary functioning kidneys. Duodenum and Pancreas Injury to the duodenum or pancreas is rare following blunt trauma, and appears to occur more incessantly in youngsters in comparability with adults. Unlike other stomach organ accidents, nearly all of recognized duodenal and pancreatic injuries would require operative exploration for repair and drainage. However, select lower grade injuries could also be amenable to profitable nonoperative management. Patients with a big intramural hematoma, significantly youngsters, may experience obstructive signs and require hospitalization for dietary management till the hematoma shrinks and obstruction resolves. Repeat imaging with oral distinction agent may be useful in these sufferers to assess the degree of luminal obstruction and resolution or progression of the lesion. The primary determinant of the need for operative intervention in pancreatic accidents would be the extent of parenchymal disruption and the presence or absence of ductal injury. Serial physical examinations and measurement of pancreatic enzymes (amylase and lipase) ought to be carried out to monitor the development or resolution of pancreatic harm and inflammation. Although hemorrhage from a missed stable organ injury has classically been described as the commonest explanation for preventable morbidity and fatality in trauma sufferers, this must be an especially rare occurrence in a contemporary, devoted trauma center. The commonest sources of morbidity in this affected person inhabitants might be these seen in any injured and hospitalized patient population. These embrace native and systemic infections, single and a quantity of organ failures, venous thromboembolism, extended hospital stay, and useful incapacity. Other issues specific to the injured organ can also be seen, similar to delayed hemorrhage, organ necrosis or abscess formation, pseudoaneurysm or arteriovenous fistula, bile or pancreatic leak, hemobilia, urinary extravasation, and end-organ ischemia from arterial or venous thrombosis. The key to optimizing patient outcomes following blunt stomach injury is anticipation of the commonly related issues, and establishment of a multidisciplinary strategy to diagnosis and administration. However, the vast majority of these complications may also be managed nonoperatively or with minimally invasive strategies. Similarly, persistent urinary extravasation can normally be handled successfully with percutaneous drainage and ureteral stent placement. Repeat imaging research should be obtained to assess the efficacy of those interventions and the timing of drain or stent removing. Parenchymal harm to any abdominal organ will result in some degree of tissue necrosis, which is often followed by tissue regeneration, reworking, or scar formation. A massive volume of necrotic tissue or necrotic tissue that turns into secondarily infected may end in native and systemic complications. Finally, vascular complications following blunt belly trauma may manifest at any time following the damage, with many being identified years later. B, Intraoperative findings demonstrate segmental space of necrosis in right hepatic lobe. Any important or symptomatic lesion is best managed by angiographic embolization. Mortality the mortality charges for nonoperative management of abdominal injuries will differ broadly by the patient population being studied, the particular organ or organs involved, and the grade of organ harm. Death in these sufferers will mostly be a results of related accidents and comorbid circumstances and never instantly attributable to the abdominal organ injury. Over half of all deaths in this patient population are attributable to different associated injuries, most commonly closed head and thoracic injuries, with solely about 10% of deaths associated to hemorrhage from the injured organ. The total mortality fee for nonoperative splenic injuries in modern sequence is approximately 6%, with the mortality rate doubling for patients older than 55 years. Failure of nonoperative management is also related to elevated mortality rates of 12% to 30%. Nonoperatively managed liver injuries are associated with higher charges of nonoperative failure, continued hemorrhage, related injuries, and thus the next general mortality price compared to splenic injuries.
Purchase 400mg zovirax mastercard
Other predictors of poor consequence are empty coronary arteries and presence of air, indicating air emboli within the coronary veins. Strict pharmacologic manipulation coupled with directly delivered countershocks of 20 to 50 J is regularly wanted to restore a normal sinus rhythm. At occasions a rhythm may be restored, however no effective pumping mechanism is noticed. Progressive myocardial dying can be witnessed, first by dilatation of the right ventricle with accompanying cessation of contractility and motion, followed by the same course of in the left ventricle. Outcomes of Emergency Department Thoracotomy for Penetrating Cardiac Injuries Wide disparity within the reporting of outcomes exists within the literature, starting from 0% to 72%. Most of these sequence are retrospective, and the patients reported have been injured due to stab wounds. Techniques for Cardiac Injury Repair Incisions Two major incisions are used in the administration of penetrating cardiac injuries. The left anterolateral thoracotomy described by Spangaro is the incision of selection within the administration of sufferers who arrive in extremis. Adjunct Maneuvers Trauma surgeons should possess several maneuvers in their armamentarium to take care of penetrating cardiothoracic accidents. This maneuver is useful to management penetrating pulmonary accidents with profuse bleeding or with a giant hematoma within the pulmonary hilum. The safe interval for this maneuver is unknown, although a 1- to 3-minute range is often quoted within the literature because the period of time after which clamps should be released. However, within the presence of acidosis, hypothermia, and ischemia, the best ventricle may not be in a position to tolerate this maneuver, leading to fibrillation and arrest. At occasions, a trauma surgeon might want to elevate the heart out of the pericardium to have the ability to repair certain accidents. If hemorrhage could be digitally controlled, gradual elevation of the guts by putting a number of laparotomy packs will enable better tolerance of this maneuver whereas decreasing the probabilities for improvement of dysrhythmias. Repair of Atrial Injuries Atrial accidents can usually be managed by placement of a Satinsky partial occlusion vascular clamp. They ought to be occluded digitally whereas simultaneously repaired by either simple interrupted or horizontal mattress sutures of Halsted. Performing cardiorrhaphy for ventricular stab wounds is often less challenging than for gunshot wounds. Missile accidents usually produce a point of blast effect that causes myocardial fibers to retract and incessantly require a number of sutures to management significant hemorrhage. Coronary Artery Injuries the restore of ventricular injuries adjoining to coronary arteries can be very difficult. Coronary arteries are usually divided into three segments: proximal, center, and distal. Injuries to the proximal and middle segments will usually require cardiopulmonary bypass for restore, and the institution of intra-aortic balloon counterpulsation followed by aortocoronary bypass, respectively. Lacerations of the distal segment of the coronary artery, significantly in the distalmost third of the vessel, are managed by ligation. Complex and Combined Injuries A vital variety of patients arrive harboring multiple associated injuries in addition to their penetrating cardiac accidents. Anatomic Location of Injury A great deal of variability exists within the literature in terms of reporting the breakdown of cardiac injuries by chambers (Table 2). Ventricular accidents happen with an incidence ranging from 37% to 67% of all cardiac injuries, whereas left ventricular injuries happen with an incidence starting from 19% to 40%. Right atrial injuries appear to happen with larger frequency ranging from 5% to 20%, whereas the left atrium, probably the most recessed chamber of the center, is injured between 2% and 12% of the time. Associated Injuries Penetrating cardiac accidents ensuing from stab wounds are usually isolated and usually solely contain one chamber because of their precordial penetration. However, missile injuries might injure the center either from precordial or from extraprecordial places, and thus have a greater propensity for inflicting multiple-chamber and associated accidents.
Syndromes
- Arterial occlusion
- Epstein-Barr virus or human herpes virus-6 (HHV-6); however, no specific virus has been identified as the cause
- Septic shock (infection throughout the body)
- Loss of bladder control
- Complement deficiencies
- Boils, painful, red bumps usually involving a hair follicle
- An overwhelming urge to make the movement
- Histiocytosis X
Buy cheapest zovirax and zovirax
Given the multiple elements that predispose these sufferers to coagulopathy, early consideration must be given to the initiation of harm management resuscitation as described in a later chapter (Torso Trauma on the Modern Battlefield), with a focus on the early administration of coagulation elements (fresh frozen plasma and cryoprecipitate) and platelets along with the usual crystalloid and packed red blood cell resuscitation. Recent literature supports the administration of blood and blood products in the ratio of 1 unit of packed red blood cells to one unit of fresh frozen plasma to one unit of platelets, and an try to minimize crystalloid resuscitation. The earliest descriptions of what subsequently became generally identified as damage control surgery concerned patients with main hepatic accidents, in whom the placement of perihepatic packing and staged operative management resulted in decreased morbidity and mortality rates. The most typical injuries that trigger a harm control approach are main liver injuries and major vascular accidents. The strategy of pack placement is of the utmost significance, and is determined by the anatomic nature of the liver harm. Major hepatic lacerations require complete mobilization of the liver, and influx occlusion at the porta hepatis (the Pringle maneuver) to reduce blood loss. Direct ligation of bleeding vessels in the depth of the laceration is critical to obtain surgical hemostasis. Once major vessel bleeding has been managed, perihepatic packs ought to be positioned anteriorly and posteriorly, compressing the liver between the 2 beds of packs and offering tamponade just like that which occurs with bimanual compression of the injured liver. Patients ought to be considered for angiography with embolization of bleeding hepatic artery branches previous to reexploration with pack elimination to assist in hemostasis (phase 3). In penetrating accidents, balloon tamponade of the missile tract, along side perihepatic packing, can be lifesaving. There are several choices out there for the administration of main vascular injuries. Many abdominal vascular accidents could be managed with easy ligation of the bleeding vessel (Table 1). These injuries are sometimes initially approached by an attempt at restore, or the placement of a temporary intraluminal shunt, with planned restore at a second operation (phase 3). Another technique for the management of exsanguinating vascular harm is the utilization of endoluminal balloon catheters to get hold of proximal and distal control of the hemorrhage. This method allows repair of the injured vessel in a comparatively dry operative field. Finally, in rare circumstances by which retrohepatic vena caval bleeding can be managed with packing, venography with endoluminal stenting stays an option. Intestinal lacerations may be controlled by suture or linear stapling or could additionally be stapled closed. If enterectomy is critical, the gastrointestinal tract is left in discontinuity, and the decision to carry out an anastomosis or stoma is postponed until the affected person has been stabilized and may return to the working room for definitive management (phase 3). Associated biliary or pancreatic accidents can often be managed with considered placement of closed suction drains, with plans to tackle the harm on the second process (phase 3). Hemodynamic instability because of splenic lacerations ought to be managed with expeditious splenectomy. Ureteral injuries identified through the damage control process ought to be stented, ligated, or drained with a percutaneous urostomy. Intraperitoneal bladder injuries must be quickly oversewn with definitive administration delayed until the second operation. The targets of temporary closure should be containment of the abdominal viscera, management of belly ascites, upkeep of tamponade on areas which were packed, and preservation of fascial integrity to help in later closure. This technique will facilitate the tamponade of bleeding whereas coagulopathy, acidosis, and hypothermia are corrected. The advantage of the Bogota bag over the vacuum-assisted techniques described next is that it permits visualization of the underlying viscera and assessment of viability, which can be essential after using shunting or ligation for a significant vascular damage. The vacuum-assisted wound coverage is constructed beginning with a nonadherent fenestrated drape placed over the viscera, followed by the applying of a sterile surgical towel. Following placement of two closed suction drains, the wound is sealed with an adhesive plastic sheet applied to the skin. The advantages of this method include upkeep of some rigidity on the belly wall fascia to decrease the chance of lack of domain and to facilitate subsequent delayed fascial closure. There are a number of commercially out there devices capable of providing similar perform.
Purchase 800 mg zovirax with visa
A two-layer closure, however a watertight, serosa-approximating single layer repair is equally acceptable. In McIntyre R, Van Stiegmann G, Eiseman B, editors: Surgical decision making, 5th ed, Philadelphia, 2004, Elsevier, pp 512�513. Although some experimental evidence suggests that the duodenal mucosa may quickly resurface over the serosal patch, this system has been fraught with complications when applied clinically. It was not utilized in any patient in the most recent multicenter trial of severe duodenal accidents, during which solely 5 sufferers (3%) had duodenoduodenostomy or duodenojejunostomy repairs. In this report of 60 sufferers with penetrating duodenal accidents, there was a 64% incidence of abdominal sepsis and a 27% death rate in 11 sufferers with duodenal gunshot wounds managed with a serosal patch or restore, compared with a 7% stomach sepsis and 0% mortality fee in 30 sufferers who had either primary repair or Roux-en-Y anastomotic repair of comparable accidents. In 17 sufferers from that same sequence with duodenal stab wounds, the complication price was additionally higher if the "sucker patch" restore of a duodenal wound was used. The "sucker patch" restore is a modification of the patch repair whereby the open end of a Roux-en-Y loop of small bowel is sutured to the duodenal defect. Buttressing the restore with omentum (my preference) or a "serosal patch" from a loop of jejunum seems logical, however the good thing about such strategies is unproved. Diversion of gastric contents is another choice, mostly completed by the Vaughan/Jordan pyloric exclusion technique. The idea is to fully divert each gastric and biliary contents away from the duodenal damage, present enteral vitamin by way of the gastrojejunostomy, and convert a possible uncontrolled lateral duodenal fistula to a managed fistula. Although as quickly as considered equally effective, the majority of these repairs fail to open, typically causing extreme problems. The gastrojejunostomy diverts gastric flow away from the duodenum for several weeks whereas the duodenal and pancreatic injuries heal. The pylorus eventually opens (2 weeks to 2 months) and the gastrojejunostomy functionally closes. In 1993, Asensio and colleagues produced a classical monograph that particulars all the surgical methods within the administration of duodenal injuries. Fang and colleagues at Chang-Gung Memorial Hospital in Taiwan have described a technical methodology of a managed launch of the pyloric exclusion knot and thereby timing the opening of the pyloric occlusion. Marginal ulceration on the web site of gastrojejunostomy has been reported in 5% to 33% of sufferers, prompting some to add truncal vagotomy to the process. The data assist the utilization of pyloric exclusion and gastrojejunostomy in "extreme" duodenal accidents or in circumstances of delayed diagnosis, although no prospective, randomized trial has proved the true good thing about gastric diversion. In addition, the added operating time and the additional anastomosis suggest a nice deal of selectivity ought to be utilized to its use. Recent research have questioned the utility of pyloric exclusion, clearly essentially the most broadly used adjunct to duodenal repair. Nassoura and Ivatury and colleagues reported on 66 sufferers with penetrating duodenal accidents managed between 1986 and 1992; 7 patients died inside forty eight hours, and of the 59 survivors, fifty six sufferers had primary restore and only three (5%) had a pyloric exclusion as an adjunct to mixed duodenal and pancreatic harm. These authors suggest use of pyloric exclusion as an adjunct to restore in patients with Penetrating Abdominal Trauma Index higher than 40 or mixed pancreatic harm, rather than using the Snyder criteria of Table 1. The presence of a pancreatic injury was present in all three sufferers (2 with primary repair only) in whom a duodenal anastomotic fistula developed, adding to the evidence of the upper risk of complication with related pancreatic injury. Similar selectivity in the utilization of pyloric exclusion is evidenced in knowledge from the National Trauma Data Bank (Dubose et al, 2008). Twentyeight patients (19%) underwent pyloric exclusion in comparability with 119 patients with primary restore. A multivariable evaluation confirmed no statistically vital difference in mortality price or incidence of septic abdominal issues between groups. Finally, Velmahos et al reviewed 193 consecutive patients at Los Angeles County Medical Center with duodenal accidents cared for between 1992 and 2004. Primary repair was carried out in 68% and pyloric exclusion as an adjunct in 32%; the pyloric exclusion group had a more extreme duodenal injury sample, more related pancreatic injuries, and more accidents to the first and second portions of the duodenum. They reported no distinction in mortality or morbidity charges between these two groups. It could be that these more modern research are displaying that adjuncts to primary restore, corresponding to pyloric exclusion, are largely pointless.
Purchase zovirax master card
Thoracic esophageal injuries are best approached by way of thoracotomy incisions primarily based on the suspected stage of the harm. Following initial studies, the choice for the incision should be determined by the presence of pleural effusion or outlined leak identified on esophagogram. Injuries to the higher two thirds of the thoracic esophagus are greatest approached via a right posterolateral thoracotomy although the fifth intercostal house. Injuries to the lower third of the thoracic esophagus are best approached through an incision within the left sixth intercostal house. Injuries to the most distal portion of the esophagus ought to be approached through a laparotomy incision, with the left side of the chest prepped into the operative area should a thoracic approach be necessitated. Additional exposure may be achieved by putting the affected person in the Trendelenburg position and by mobilizing the left lobe of the liver. The midline incision can be extended superiorly and to the left of the xiphoid process for an extra 1 to 2 cm of exposure. The esophagus ought to be exposed with blunt guide dissection on the gastroesophageal junction and encircled with a Penrose drain. The hiatus can be widened, if necessary, to expose wounds close to the gastroesophageal junction. Small injuries may be closed transversely, whereas injuries larger than 2 to three cm may be closed longitudinally so as to avoid undue rigidity. Unfortunately, diagnostic delay often yields significant mediastinal inflammation and sepsis. Furthermore, the shortage of a serosal layer complicates main reapproximation because the esophageal tissues are extremely friable especially underneath these circumstances. Numerous methods have been proposed including nonoperative administration with drainage, esophageal resection, and diversion with exclusion. The use of pleural and pericardial flaps has been broadly described for buttressing primary repairs. More recently, numerous muscle flaps have been advocated for main repair of esophageal defects. However, adequate esophageal tissue d�bridement, tension-free repairs, and efficient drainage stay the mainstays of profitable operative management. The paraesophageal and precervical planes should also be inspected, irrigated, and drained to decrease contamination. We have treated several patients with massive defects that could not be closed primarily with muscle flaps. These accidents are incessantly associated with acute coagulation necrosis, diffuse tissue hemorrhage, and vital irritation. Occasionally, the irritation is so severe that the defect is tough to determine. Both mucosal and muscular layers ought to be recognized, and one should acknowledge that the mucosal tear is usually bigger than the muscular defect. Failure to completely expose the mucosal defect might end in incomplete closure and subsequent leakage from the site of repair. If potential, a double-layered closure must be carried out with reapproximation of both mucosa and muscularis. The restore ought to at all times be buttressed with adjacent tissue for additional reinforcement. Primary repairs of the thoracic esophagus are most likely to fail in a big share of cases. The lower esophageal blood supply and the dearth of a serosal layer make major closure rather more tenuous. As a end result, several adjoining tissues have been used to buttress or primarily restore these accidents with variable success. Pleural flaps have been extensively used but are sometimes too friable and generally provide inadequate tissue coverage. Pleural flaps are more dependable if there have been inflammatory adjustments to thicken the pleura. The use of pericardial flaps seems unwise, as this would expose the pericardial sac to contamination. Adequate tissue coverage is very essential in close proximity to the trachea in order to scale back the incidence of later fistula development.
Purchase line zovirax
Thus, though bronchial rupture may be treated successfully within the acute or the delayed part, early diagnosis and remedy reduce the chance of infection and different issues. Although unusual, tracheobronchial accidents shall be encountered at most busy centers. These are difficult circumstances in which consequence is decided by successful initial airway management as properly as the extent of suspicion by the astute clinician in investigating sufferers with indicators and symptoms of the injury. With well-thought-out airway administration and early operative intervention, good outcomes could be expected generally. Asensio, Patrizio Petrone, Alejandro Perez-Alonso, Thomas Templin, Shreya Shetty, Gerd Daniel Pust, Kirby R. Ancient Greek chronicles reveal examples of penetrating chest wounds and pulmonary accidents; the Greeks had anatomic knowledge and had been cognizant of the thoracic buildings and the position of the lungs contained in the hemithoracic cavities. Although the success of those early therapy modalities stays unknown, it appears that throughout Olympic competitions, physicians in historic Greece had been at least capable of determine potentially lethal chest injuries, and most likely try their treatment. Pausanias, a Greek traveler in the course of the height of Roman rule, described a penetrating injury to the chest, inflicted to Creugas of Epidamnus by Damoxenos of Syracuse, with the presence of what appears to be an obvious pulmonary harm. Eusebius described in Evangelical Preparation, the match of Cleomedes of Astypalaia in opposition to Ikkos of Epidauros: "Why did they deify Cleomedes A description of a lung injury was found in a treatise of Theodoric in 1226: "[W]hile I was residing in Bolonia, a certain Domicellus, a Bolognan of regular start was, cured by the hand of Master Hugo, part of his lung being torn away and Master Roand was there to witness it. In 1635, Alvar Nu�ez Cabeza de Vaca, a Spaniard, whereas traveling from the Mexican northern territory to the capital of Nueva C Espa�a (Mexico City), was captured by Indians. His innovation in surgical administration gained freedom from his captors for him and his good friend. During the 16th century, a few contributions have been made to the management of traumatic pulmonary accidents. Ambroise Par� treated penetrating thoracic accidents by placing a scalding mixture of oil and treacle within the wound as the first dressing. In Germany, Auenbrugger mentioned: "opening the chest triggered asphyxia as a outcome of the lung collapsed. In the 1840s, the French Academy of Medicine studied the treatment of empyema to produce guidelines for its therapy based on warfare experiences. In the 18th century, Hewson known as attention to the mechanism of pulmonary rupture after blunt trauma to the chest, and in 1886, Ashurt described rupture of thoracic viscera with out rib fractures. These incisions remain important contributions to the trauma surgical armamentarium to manage traumatic pulmonary injuries. The remedy of thoracic wounds in World War I started with many of the fundamental rules described within the 19th century. However, when surgical procedure was required for thoracic harm, it was aggressive and largely profitable following ideas of hermetic closure for wounds and elimination of foreign our bodies. In distinction to their surgical counterparts within the German Army, American surgeons with the Allied Expeditionary Force used positive-pressure anesthesia and a nitrous oxide/ oxygen combination, while working towards early thoracotomies following the ideas for good exposure injuries, resection of affected anatomic constructions, suture ligature, and irrigation of the thoracic cavity. Thoracotomies were closed hermetic, traumatic wounds excised, and no drains were positioned. During this time Grey-Turner, Miles, Gask, Duval, and Bastianelli outlined the technique of pulmonary decortication for the treatment of retained hemothorax after traumatic lung injuries (White). Thoracentesis was used repeatedly until the thoracic cavity was totally evacuated. The injured lung was allowed to reexpand and tamponade bleeding, in hopes of returning pulmonary function to normal levels. Water-sealed intercostal catheters had been placed in patients with tension pneumothoraces. Thoracotomy was reserved for continued hemorrhage or vital air leaks; extra indications included thoracoabdominal wounds, mediastinal injuries, traumatic thoracotomy, "the sucking chest wound," and removal of international our bodies. Overall mortality rate with this therapy of struggle chest wounds was reported as 8%. Conservative administration of traumatic hemothorax was thus a therapeutic strategy extraordinarily suited to these conditions. Eighty percent of casualties from the Korean War have been managed by repeated thoracentesis alone; nonetheless, there was restricted experience with using chest tubes for drainage of hemothorax.
Buy zovirax 200mg mastercard
Recently, a quantity of exterior gadgets in addition to indwelling catheters have been developed to facilitate systemic rewarming. Invasive monitoring, including central venous stress monitoring or Swan-Ganz monitoring, could additionally be essential in the quick postoperative interval to information resuscitative efforts. Alternatively, noninvasive measures of cardiac output could also be used to guide resuscitative measures. An anion gap can be utilized to differentiate lactic acidosis from hyperchloremic acidosis. Hyperchloremic acidosis leads to a narrowed anion gap, and lactic acidosis leads to a widened anion hole. Although correction of acidosis and hypothermia will help within the correction of the coagulopathy seen after damage control procedures, these patients will require ongoing transfusion of recent frozen plasma, cryoprecipitate, and platelets, or ongoing harm control resuscitation. All merchandise should be delivered by way of fluid warmers to reduce the time to rewarming. There is extensive literature indicating that the timing of definitive orthopedic stabilization ought to be delayed longer than 72 hours. A statistically significant improve in multisystem organ dysfunction has been reported in patients undergoing stabilization at 2 to four days in comparability with these patients who had their fractures stabilized at 6 to 8 days. The timing of reoperation has not been standardized, but most trauma surgeons will return to the operating room inside 48 to seventy two hours, as reexploration prior to seventy two hours is associated with decreased rates of morbidity and mortality. During reexploration, a formal exploration is carried out to determine any injuries that will have been missed through the injury management procedure. Consideration should be given to delayed main closure of the belly wall fascia, though this is in all probability not feasible if important edema persists. Most sufferers (80%) can have their fascia primarily closed within 5 to 7 days of damage. Velcro closure devices may be employed and may find yourself in main fascial closure up to 21 days following injury. Delayed restore of this deliberate ventral hernia can then happen after 6 to 12 months. Following injury management thoracotomy, the patient might safely be returned to the operating room after correction of all physiologic derangements. Measurement of intravesical bladder strain via a Foley catheter can be used as a surrogate for the intraabdominal strain. A pressure greater than 25 mm Hg with evidence of physiologic compromise mandates stomach decompression. Alternatively, an belly perfusion strain could also be decided (mean arterial stress minus intraabdominal pressure); decompression should be performed for belly perfusion pressures lower than 60 mm Hg. After decompressing the abdomen, there should be a direct improvement in visceral perfusion, renal perfusion, cardiac operate, and ventilatory mechanics. Unplanned reoperation may be needed within the patient with ongoing postoperative hemorrhage despite aggressive resuscitation and correction of the lethal triad. Indications for return to the working room within the first 24 hours after a harm control procedure are listed in Box 2. These patients will require belly wall reconstruction on the time of fistula takedown. Damage management allows life-threatening points to be addressed expeditiously during truncated operative procedures. The ability to stage the definitive surgical procedure permits correction of the lethal triad of hypothermia, coagulopathy, and acidosis and leads to improved survival in patients who previously would have died of their accidents. Miller C urrent critical care supportive measures make it attainable for patients with extreme accidents and physiologic impairment to survive what in any other case may need been deadly conditions. One of the main surgical penalties of intensive resuscitation efforts regards the situation of the abdominal wall. Although the objective must be to always shut the stomach following laparotomy, main closure could additionally be technically impossible or deleterious owing to any number of circumstances. The chapter will conclude with a discussion of special issues of the open abdomen, together with stomach wall reconstruction, nutritional assist, and outcomes.
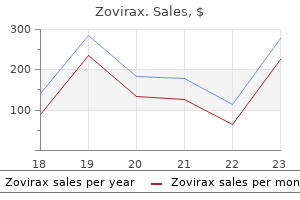
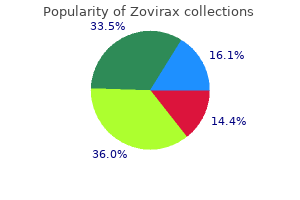
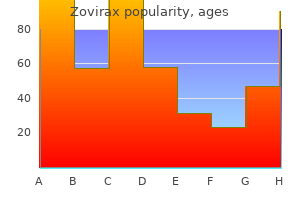
Real Experiences: Customer Reviews on Zovirax
Ballock, 51 years: Hemorrhage from blunt harm is rare however might occur secondary to associated orthopedic injuries resulting in partial or full laceration or transection of the vessel. The traits of each illness and its agent shall be presented with emphasis positioned on detection, diagnosis, remedy, precautions, prophylaxis, quarantine, decontamination, and necrology (Tables 1 to 3). If the stress normalizes by this step alone, cutting the upper canthal tendon could be deferred. This evaluation contains an analysis of the patient for life-threatening conditions that must be promptly addressed.
Larson, 60 years: The most common main complication is rehemorrhage (11%), which often requires reembolization or surgical splenectomy. The commonest symptoms and indicators are hemoptysis and hypoxia leading to dyspnea, tachypnea, and poor compliance. Regardless of specific technique, endovascular surgery for such accidents should adhere to related vascular trauma dogma as open surgery. By 1994, intentional harm was the 10th main explanation for demise in America (20,000 per year) and the main reason for premature dying.
Yussuf, 32 years: Whereas many collection have selected physiologic parameters as predictors of end result, none have statistically validated their predictive values. Other mechanisms such as impalement and shotgun wounds are reported with a decrease frequency of 1% to 5% of cases. Once an air leak occurs, management is determined by timing (less than or greater than 7 days postoperatively), diploma (ventilatory compromise and whether or not the defect can be visualized endoscopically), physiologic status, and whether or not or not the affected person is ventilated. Five minutes of compression with lap pads is performed after the application of a topical agent to the uncooked surface.
Rocko, 63 years: Randomized, controlled investigations have to be carried out to present proof to assist dictate the use of blood in critically unwell trauma sufferers. This will enable for dissection of the origin of the carotid arteries off the arch of the aorta and within the case of a proper widespread carotid artery, off the brachiocephalic trunk. Thoracic endoscopy in this setting is playing an more and more important role in early prognosis and therapy for these complications, and probably enhancing consequence. The advanced and complicated architecture of the midface is organized in horizontal beams and vertical buttresses that facilitate the transfer and distribution of forces to other areas of the maxillofacial area and cranium base.
Onatas, 62 years: Auscultation in trauma has a high specificity however very poor sensitivity, so focus should be placed only on the presence and symmetry of air entry. There are actually no evidenced-based recommendations for the suitable use of covered stents for traumatic injuries presently. Therefore, the use of a buttress usually enhances healing with out fistula development. Lacerations or partial transections to the common or external iliac arteries may be repaired primarily with a 4-0 or 5-0 Prolene suture in either interrupted or working style.
Masil, 47 years: It was postulated that the flexibility to predict the onset of coagulopathy would have vital implications for instituting harm management. The majority (85%) of midshaft clavicular fractures will heal without intervention, and preliminary management consists of immobilization with a figure-of-eight dressing or shoulder immobilizer. All chest tubes have been removed within 48 hours, and 9 patients were discharged home in seventy two hours. Paul et al in 2010 evaluated their earlier work on abdominal vascular accidents and in contrast it with their most up-to-date experience.
Spike, 59 years: Intracompartmental pressure measurements could additionally be helpful in deciding borderline circumstances, but in general, the analysis is made on scientific grounds. Most patients with blunt hepatic trauma have associated accidents, both intra-abdominal and extraabdominal. The surgical armamentarium to manage the penetrating pulmonary injuries discussed subsequent is organized into two broad classes: tissue-sparing techniques and resectional procedures. State-of-the-art multislice scanners not only present improved temporal and spatial decision, however can purchase complete physique photographs in lower than 1.
10 of 10 - Review by K. Faesul
Votes: 335 votes
Total customer reviews: 335


