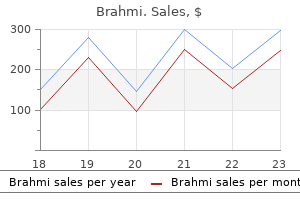
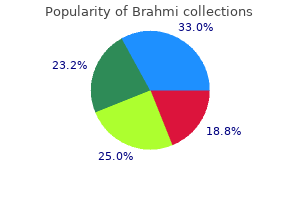
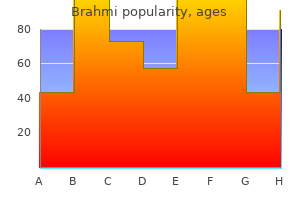
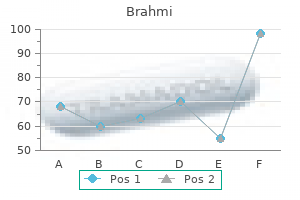
Brahmi dosages: 60 caps
Brahmi packs: 1 packs, 2 packs, 3 packs, 4 packs, 5 packs, 6 packs, 7 packs, 8 packs, 9 packs, 10 packs

Generic 60caps brahmi with amex
They can also lean on their knees or on the arms of a chair to repair their pectoral girdle, so these muscle tissue are in a place to act on their rib attachments and expand the thorax. Extrapleural Access Intrathoracic Surgical Fixation makes it difficult to appreciate in the embalmed cadaver, however in surgical procedure, the comparatively unfastened nature of the thin endothoracic fascia supplies a natural cleavage aircraft, permitting the surgeon to separate the costal parietal pleura lining the lung cavity from the thoracic wall. Herpes Zoster Infection of Spinal Ganglia Herpes zoster causes a classic, dermatomally distributed skin lesion-shingles -an agonizingly painful condition. After invading a ganglion, the virus produces a pointy burning pain in the dermatome equipped by the involved nerve. Although primarily a sensory neuropathy (pathological change in a nerve), weak spot from motor involvement happens in zero. Muscular weak spot normally occurs in the same myotomal distribution, as do the dermatomal ache and vesicular eruptions. Vaccination confers protection in opposition to herpes zoster and is really helpful for individuals aged 60 years and older. Intercostal Nerve Block Local anesthesia of an intercostal area is produced by injecting an anesthetic agent around the intercostal nerves between the paravertebral line and the realm of required anesthesia. This procedure, an intercostal nerve block, is usually utilized in sufferers with rib fractures and sometimes after thoracic surgery. It includes infiltration of the anesthetic across the intercostal nerve trunk and its collateral branches. The term block signifies that the nerve endings in the pores and skin and transmission of impulses via the sensory nerves carrying details about ache are interrupted (blocked) before the impulses reach the spinal wire and brain. Because any particular area of pores and skin often receives innervation from two adjoining nerves, appreciable overlapping of contiguous dermatomes happens. The muscle tissue which are actually thoracic, however, present few if any floor features. The costal muscular tissues perform primarily to assist (provide tonus for) the intercostal spaces, resisting unfavorable and constructive intrathoracic pressures. Neurovasculature of thoracic wall: the pattern of distribution of neurovascular buildings to the thoracic wall reflects the construction of the thoracic cage. Breasts the breasts are probably the most outstanding superficial constructions in the anterior thoracic wall, particularly in girls. The mammary glands are within the subcutaneous tissue overlying the pectoralis major and minor muscles. At the greatest prominence of the breast is the nipple, surrounded by a circular pigmented space of pores and skin, the areola (L. The superior two thirds of the determine demonstrates the suspensory ligaments and alveoli of the breast with resting lobules of mammary gland; the inferior part exhibits lactating lobules of mammary gland. They are rudimentary and functionless in males, consisting of just a few small ducts or epithelial cords. The roughly circular physique of the feminine breast rests on a mattress of the breast that extends transversely from the lateral border of the sternum to the midaxillary line and vertically from the 2nd via sixth ribs. Two thirds of the mattress are fashioned by the pectoral fascia overlying the pectoralis major and the other third by the fascia covering the serratus anterior. Between the breast and the pectoral fascia is a free subcutaneous tissue airplane or potential space-the retromammary space (bursa). This aircraft, containing a small quantity of fats, allows the breast a point of movement on the pectoral fascia. A smaller a half of the mammary gland could lengthen along the inferolateral fringe of 774 the pectoralis major toward the axillary fossa (armpit), forming an axillary process or tail (of Spence). The mammary glands are firmly attached to the dermis of the overlying pores and skin by substantial skin ligaments (L. These condensations of fibrous connective tissue, notably nicely developed in the superior a part of the gland, help assist the lobes and lobules of the mammary gland. During puberty (ages 8�15 years), the female breasts normally enlarge, owing in part to glandular improvement but primarily from elevated fat deposition. Breast size and shape are determined partly by genetic, ethnic, and dietary elements. The lactiferous ducts give rise to buds that become 15�20 lobules of the mammary gland, which constitute the parenchyma (functional substance) of the mammary gland.
Buy brahmi 60caps line
The many arteries making up the peri-articular anastomosis across the knee provide an important collateral circulation for bypassing the popliteal artery when the knee joint has been maintained too lengthy in a fully flexed position or when the vessels are narrowed or occluded. Five genicular branches of the popliteal artery provide the capsule and 1702 ligaments of the knee joint. The genicular arteries are the superior lateral, superior medial, middle, inferior lateral, and inferior medial genicular arteries. They participate within the formation of the peri-articular genicular anastomosis, a community of vessels surrounding the knee that gives collateral circulation capable of sustaining blood provide to the leg during full knee flexion, which may kink the popliteal artery. Other contributors to this important genicular anastomosis are the descending genicular artery, a department of the femoral artery, superomedially. Muscular branches of the popliteal artery supply the hamstring, gastrocnemius, soleus, and plantaris muscles. The superior muscular branches of the popliteal artery have clinically essential anastomoses with the terminal part of the profunda femoris and gluteal arteries. The popliteal vein begins at the distal border of the popliteus as a continuation of the posterior tibial vein. Throughout its course, the vein lies close to the popliteal artery, lying superficial to it in the identical fibrous sheath. More superiorly, the popliteal vein lies posterior to the artery, between this vessel and the overlying tibial nerve. Superiorly, the popliteal vein, which has several valves, becomes the femoral vein because it traverses the adductor hiatus. The small saphenous vein passes from the posterior side of the lateral malleolus to the popliteal fossa, the place it pierces the deep popliteal fascia and enters the popliteal vein. The superficial popliteal lymph nodes are normally small and lie within the subcutaneous tissue. A lymph node lies on the termination of the small saphenous vein and receives lymph from the lymphatic vessels that accompany this vein. The deep popliteal lymph nodes surround the vessels and obtain lymph from the joint capsule of the knee and the lymphatic vessels that accompany the deep veins of the leg. The lymphatic vessels from the popliteal lymph nodes follow the femoral vessels to the deep inguinal lymph nodes. The anterior (dorsiflexor or extensor) compartment accommodates 4 muscle tissue (the fibularis tertius lies inferior to the level of this section). The posterior (plantarflexor or flexor) compartment, containing seven muscles, is subdivided by an intracompartmental transverse intermuscular septum right into a superficial group of three (two of which are generally tendinous/aponeurotic at this level) and a deep group of 4. The popliteus (part of the deep group) lies superior to the level of this section. The anterior compartment of the leg, or dorsiflexor (extensor) compartment, is positioned anterior to the interosseous membrane, between the lateral floor of the shaft of the tibia and the medial surface of the shaft of the fibula. The anterior compartment is bounded anteriorly by the deep fascia of the leg and skin. The deep fascia overlying the anterior compartment is dense superiorly, providing a part of the proximal attachment of the muscle instantly deep to it. With unyielding structures on three sides (the two bones and the interosseous membrane) and a dense fascia on the remaining facet, the relatively small anterior compartment is particularly confined and due to this fact most susceptible to compartment syndromes (see the medical box "Containment and Spread of Compartmental Infections in the Leg"). Inferiorly, two band-like thickenings of the fascia type retinacula that bind the tendons of the anterior compartment muscle tissue before and after they cross the ankle joint, stopping them from bowstringing anteriorly during dorsiflexion of the joint. These dissections demonstrate the continuation of the anterior and lateral leg muscle tissue into the foot. The thinner parts of the deep fascia of the leg have been removed, leaving the thicker parts that make up the extensor and fibular retinacula, which retain the tendons as they cross the ankle. At the ankle, the vessels and the deep fibular nerve lie halfway between the malleoli and between the tendons of the long dorsiflexors of the toes. Synovial sheaths surround the tendons as they cross beneath the retinacula of the ankle.
Buy generic brahmi line
The relatively large measurement of the buccal fat-pads in infants prevents collapse of the cheeks throughout sucking and produces their chubby-cheeked look. The ethmoid bone, orbital cavities, and superior parts of the nasal cavities have almost completed their development by the seventh year. Expansion of the orbits and development of the nasal septum carry the maxillae infero-anteriorly. Considerable facial progress happens during childhood because the paranasal sinuses develop and permanent teeth erupt. Our interactions with others happen largely by way of the face (including the ears) and thus the time period interface for a website of interactions. Whereas the shape and features of the face present our identification, much of our effect on others and their perceptions about us result from the way we use facial muscles to make the slight alterations within the options that constitute facial features. Scalp the scalp consists of pores and skin (normally hair bearing) and subcutaneous tissue that cover the neurocranium from the superior nuchal strains on the occipital bone to the supra-orbital margins of the frontal bone. The scalp is composed of 5 layers, the primary three of which are linked intimately and move as a unit. The skin is certain tightly to the epicranial aponeurosis, which moves freely over the pericranium and cranium because of the intervening unfastened connective tissue. Aponeurosis refers to the epicranial aponeurosis, the flat intermediate tendon of the occipitofrontalis muscle. Innervation of the 2 bellies by the posterior auricular and temporal branches of the facial nerve is demonstrated. Skin: thin, except within the occipital region, contains many sweat and sebaceous glands and hair follicles. Aponeurosis (epicranial aponeurosis): the broad, robust, tendinous sheet that covers the calvaria and serves because the attachment for muscle bellies converging from the brow and occiput (occipitofrontalis muscle). The frontal stomach of the occipitofrontalis pulls the scalp anteriorly, wrinkles the brow, and elevates the eyebrows. The occipital belly of the occipitofrontalis pulls the scalp posteriorly, smoothing the pores and skin of the brow. The superior auricular muscle (a specialized posterior a part of the temporoparietalis) elevates the auricle of the external ear. All components of the epicranius (muscle and aponeurosis) are innervated by the facial nerve. Loose areolar tissue: a sponge-like layer together with potential spaces that will distend with fluid on account of harm or an infection. This layer permits free motion of the scalp proper (the first three layers-skin, connective tissue, and epicranial aponeurosis) over the underlying calvaria. Pericranium: a dense layer of connective tissue that types the external periosteum of the neurocranium. It is firmly hooked up however may be stripped from the crania of dwelling individuals, besides where the pericranium is continuous with the fibrous tissue in the cranial sutures. Muscles of Face and Scalp the facial muscle tissue (muscles of facial expression) are in the subcutaneous tissue of the anterior and posterior scalp, face, and neck. Most muscles connect to bone or fascia and produce their results by pulling the pores and skin. All muscular tissues of facial expression develop from mesoderm in the second pharyngeal arches. The muscular sheet differentiates into muscles that encompass the facial orifices (mouth, eyes, and nose), serving as sphincter and dilator mechanisms that additionally produce many facial expressions. Because of their widespread embryological origin, the platysma and facial muscular tissues are often fused, and their fibers are regularly intermingled. These muscular tissues are superficial sphincters and dilators of the orifices of the top. Because the aponeurosis is a layer of the scalp, unbiased contraction of the occipital belly retracts the scalp and contraction 1927 of the frontal belly protracts it. Acting simultaneously, the occipital belly, with bony attachments, works as a synergist with the frontal stomach, which has no bony attachments, to elevate the eyebrows and produce transverse wrinkles across the brow. In addition, we add emphasis to our vocal communication with our facial expressions. Several muscular tissues alter the form of the mouth and lips during talking in addition to during such actions as singing, whistling, and mimicry.
Purchase 60 caps brahmi fast delivery
The proximal digital crease of the thumb crosses obliquely, at or proximal to the first metacarpophalangeal joint. The pores and skin ridges on the pulp (pads) of the digits, forming the fingerprints, are used for identification because of their unique patterns. The physiological perform of the pores and skin ridges is to reduce slippage when greedy objects. The 637 fibrous degeneration of the longitudinal bands of the palmar aponeurosis on the medial side of the hand pulls the 4th and 5th fingers into partial flexion on the metacarpophalangeal and proximal interphalangeal joints. Gradually, progressive contracture of the longitudinal bands produces raised ridges in the palmar skin that reach from the proximal a half of the hand to the bottom of the 4th and 5th fingers. Treatment of Dupuytren contracture often entails surgical excision of all fibrotic components of the palmar fascia to free the fingers (Salter, 1999). Hand Infections Because the palmar fascia is thick and strong, swellings resulting from hand infections usually seem on the dorsum of the hand, where the fascia is thinner. The potential fascial areas of the palm are important as a end result of they could turn out to be contaminated. The fascial areas decide the extent and path of the spread of pus shaped by these infections. Depending on the site of infection, pus will accumulate within the thenar, hypothenar, midpalmar, or adductor compartments. Antibiotic therapy has made infections that spread beyond one of these fascial compartments uncommon; nevertheless, an untreated infection can spread proximally from the midpalmar space via the carpal tunnel into the forearm, anterior to the pronator quadratus and its fascia. Tenosynovitis Injuries similar to a puncture of a finger by a rusty nail can cause infection of the digital synovial sheaths. When irritation of the tendon and synovial sheath occurs (tenosynovitis), the digit swells and movement becomes painful. Because the tendons of the 2nd, 3rd, and 4th fingers practically always have separate synovial sheaths, the infection is normally confined to the infected finger. If the infection is untreated, nonetheless, the proximal ends of these sheaths could rupture, allowing the an infection to unfold to the midpalmar area. Because the synovial sheath of the little finger is normally steady with the frequent flexor sheath. How far an an infection spreads from the fingers is decided by variations of their connections with the widespread flexor sheath. Excessive friction of those tendons on their common sheath leads to fibrous thickening of the sheath and stenosis of the osseofibrous tunnel. The excessive friction is attributable to repetitive forceful use of the arms throughout gripping and wringing. This condition, known as Quervain tenovaginitis stenosans, causes pain in the wrist that radiates proximally to the forearm and distally towards the thumb. Local tenderness is felt over the common flexor sheath on the lateral side of the wrist. Thickening of a fibrous digital sheath on the palmar aspect of the digit produces stenosis of the osseofibrous tunnel, the outcome of repetitive forceful use of the fingers. This situation is identified as digital tenovaginitis stenosans (trigger finger or snapping finger). Laceration of Palmar Arches Bleeding is usually profuse when the palmar (arterial) arches are lacerated. It 641 will not be sufficient to ligate only one forearm artery when the arches are lacerated, because these vessels usually have numerous communications within the forearm and hand and thus bleed from both ends. To obtain a bloodless surgical operating area for treating complicated hand accidents, it may be essential to compress the brachial artery and its branches proximal to the elbow. This procedure prevents blood from reaching the ulnar and radial arteries via the anastomoses around the elbow. Ischemia of Digits (Fingers) Intermittent bilateral attacks of ischemia of the digits, marked by cyanosis and sometimes accompanied by paresthesia and pain, are characteristically introduced on by chilly and emotional stimuli. Postsynaptic fibers from the sympathetic ganglia enter nerves that kind the brachial plexus and are distributed to the digital arteries by way of branches arising from the plexus.
Discount brahmi 60 caps with mastercard
When standing with the knees locked in the fully prolonged position, the popliteus acts to rotate the femur laterally 5� on the tibial plateaus, releasing the knee from its close-packed or locked position so that flexion can occur. When the foot is off the bottom and the knee is flexed, the popliteus can help the medial hamstrings (the "semi-muscles") in rotating the tibia medially beneath the femoral condyles. When barefoot, this thrust is delivered by the good toe; however with soled footwear on, it becomes a part of the thrust of plantarflexion delivered by the forefoot. The tendon then crosses deep to the tendon of the flexor digitorum longus within the sole of the foot. These bones defend the tendon from the strain of the pinnacle of the 1st metatarsal bone. While standing (especially on one foot), however, the two muscles might cooperate to depress the lateral side of the foot and pull medially on the leg as needed to counteract lateral leaning for balance. It runs vertically through the popliteal fossa with the popliteal artery, passing between the heads of the gastrocnemius, the 2 constructions exiting the fossa by passing deep to the tendinous arch of the soleus. Postero-inferior to the medial malleolus, the tibial nerve divides into the medial and lateral plantar nerves. A department of the tibial nerve, the medial sural cutaneous nerve, is usually joined by the sural communicating branch of the common fibular nerve to kind the sural nerve. The sural nerve provides the pores and skin of the lateral and posterior a part of the inferior third of the leg and the lateral side of the foot. It begins on the distal border of the popliteus, as the popliteal artery passes deep to the tendinous arch of the soleus and simultaneously bifurcates into its terminal branches. Close to its origin, the posterior tibial artery gives rise to its largest department, the fibular artery, which runs lateral and parallel to it, also inside the deep subcompartment. During its descent, the posterior tibial artery is accompanied by the tibial nerve and veins. Deep to the flexor retinaculum and the origin of the abductor hallucis, the posterior tibial artery divides into medial and lateral plantar arteries, the arteries of the sole of the foot. The fibular (peroneal) artery, the largest and most necessary branch of the posterior tibial artery, arises inferior to the distal border of the popliteus and the tendinous arch of the soleus. The fibular artery gives muscular branches to the popliteus and different muscular tissues in both the posterior and the lateral compartments of the leg. Distally, the fibular artery provides rise to a perforating branch and terminal lateral malleolar and calcaneal branches. The perforating branch pierces the interosseous membrane and passes to the dorsum of the foot, where it anastomoses with the arcuate artery. The lateral calcaneal branches supply the heel, and the lateral malleolar branch joins other malleolar branches to type a peri-articular arterial anastomosis of the ankle. The circumflex fibular artery arises from the origin of the anterior or posterior tibial artery on the knee and passes laterally over the neck of the fibula to the anastomoses around the knee. It pierces the tibialis posterior, to which it supplies branches, and enters the nutrient foramen within the proximal third of the posterior floor of the tibia. Surface Anatomy of Leg the tibial tuberosity is an easily palpable elevation on the anterior side of the proximal a half of the tibia, approximately 5 cm distal to the apex of the patella. This oval elevation indicates the extent of the head of the fibula and the bifurcation of the popliteal artery into the anterior and posterior tibial arteries. Extensors and flexors of toes are being contracted concurrently, demonstrating extensor tendons without elevating toes from ground. The patellar ligament could additionally be felt because it extends from the inferior border of the 1734 apex of the patella. When the knee flexes to a proper angle, a despair could additionally be felt on both sides of the patellar ligament. The head of the fibula is subcutaneous and may be palpated at the posterolateral aspect of the knee, on the level of the tibial tuberosity. The tendon of the biceps femoris could additionally be traced by palpating its distal attachment to the lateral aspect of the top of the fibula. This tendon and the head and neck of the fibula guide the analyzing finger to the common fibular nerve. The nerve is indicated by a line along the biceps femoris tendon, posterior to the pinnacle of the fibula, and around the lateral aspect of the fibular neck to its anterior side, simply distal to the fibular head. The anterior border of the tibia is sharp, subcutaneous, and easily followed distally by palpation from the tibial tuberosity to the medial malleolus.

Order brahmi cheap
The posterior lymphatic vessels pass posterior to the top of the pancreas and drain into the superior mesenteric lymph nodes. Efferent lymphatic vessels from the duodenal lymph nodes drain into the celiac lymph nodes. The shut positional relationship of those organs results in sharing of blood vessels, lymphatic vessels, and nerve pathways, in whole or partially. The nerves of the duodenum derive from the vagus and greater and lesser (abdominopelvic) splanchnic nerves by the use of the celiac and superior mesenteric plexuses. The nerves are next conveyed to the duodenum by way of periarterial plexuses extending to the pancreaticoduodenal arteries (see also "Summary of the Innervation of Abdominal Viscera," p. The third a part of the small intestine, the ileum, ends on the ileocecal junction, the union of the terminal ileum and the cecum. Together, the jejunum and ileum are 6�7 m long, the jejunum constituting approximately two fifths and the ileum roughly three fifths of the intraperitoneal section of the small gut. The terminal ileum normally lies in the pelvis from which it ascends, ending within the medial side of the cecum. Structure of the mesentery and small gut: distinctive options of the jejunum and ileum. The mesentery is a double-layered fold of visceral peritoneum that suspends the intestine and conducts neurovasculature from the posterior body wall. The mesentery is a fan-shaped fold of peritoneum that attaches the jejunum and ileum to the posterior stomach wall. The origin or root of the mesentery (approximately 15 cm long) is directed obliquely, inferiorly, and to the best. It extends from the duodenojejunal junction on the left facet of vertebra L2 to the ileocolic junction and the proper sacro-iliac joint. The average length of the mesentery from its root to the intestinal border is 20 cm. Between the two layers of the mesentery are the superior mesenteric vessels, lymph nodes, a variable amount of fats, and autonomic nerves. The transverse and sigmoid mesocolons and the mesentery of the jejunum and ileum 1101 have been minimize at their roots. The ileocolic and right colic arteries on the best facet and the left colic and sigmoid arteries on the left aspect originally coursed inside mesenteries (ascending and descending mesocolons) that later fused to the posterior wall; they can be re-established surgically. The arteries unite to kind loops or arches, known as arterial arcades, which give rise to straight arteries, called vasa recta. Specialized lymphatic vessels within the intestinal villi (tiny projections of the mucous membrane) that absorb fats are referred to as lacteals. They empty their milklike fluid into the lymphatic plexuses in the walls of the jejunum and ileum. The lacteals drain in turn into lymphatic vessels between the layers of the mesentery. Within the mesentery, the lymph passes sequentially through three teams of lymph nodes. The superior nodes form a system by which the central nodes, on the root of the superior mesenteric artery, obtain lymph from the mesenteric, ileocolic, right colic, and middle colic nodes, which in flip obtain lymph from juxta-intestinal lymph nodes. Efferent lymphatic vessels from the mesenteric lymph nodes drain to the 1103 superior mesenteric lymph nodes. Lymphatic vessels from the terminal ileum follow the ileal branch of the ileocolic artery to the ileocolic lymph nodes. The sympathetic fibers in the nerves to the jejunum and ileum originate in the T8�T10 segments of the spinal cord and reach the superior mesenteric nerve plexus by way of the sympathetic trunks and thoracic abdominopelvic (greater, lesser, and least) splanchnic nerves. The presynaptic sympathetic fibers synapse on cell our bodies of postsynaptic sympathetic neurons within the celiac and superior mesenteric (prevertebral) ganglia. The parasympathetic fibers within the nerves to the jejunum and ileum derive from the posterior vagal trunks. The presynaptic parasympathetic fibers synapse with postsynaptic parasympathetic neurons in the myenteric and submucosal plexuses of the enteric nervous system within the intestinal wall (see additionally "Summary of Innervation of Abdominal Viscera," p. Presynaptic sympathetic nerve fibers originate in the T8 or T9 through T10 or T11 segments of the spinal twine and attain the celiac plexus by way of the sympathetic trunks and greater and lesser (abdominopelvic) splanchnic nerves. After synapsing in the celiac and superior mesenteric ganglia, postsynaptic nerve fibers accompany the arteries to the gut. Presynaptic parasympathetic (vagus) nerves originate in the medulla (oblongata) and pass to the gut through the posterior 1105 vagal trunk.

Order brahmi 60caps online
Chronic encephalitis associated with epilepsy: immunohistochemical and ultrastructural studies. Genetic regulatory elements introduced into neural stem and progenitor cell populations. Hydrocephalus due to cerebrospinal fluid overproduction by bilateral choroid plexus papillomas. Isolation and characterization of tumorigenic, stemlike neural precursors from human glioblastoma. Phosphorylation of neurofilament H subunit as related to association of neurofilaments. Innate (inherent) control of brain an infection, mind inflammation and brain restore: the role of microglia, astrocytes, "protecting" glial stem cells and stromal ependymal cells. Acute transplantation of glial-restricted precursor cells into spinal cord contusion injuries: survival, differentiation, and effects on lesion surroundings and axonal regeneration. Organization of mammalian neurofilament polypeptides throughout the neuronal cytoskeleton. Localization of regions mediating the Cushing response in the central nervous system of the cat. X-linked aqueductal stenosis: scientific and neuropathological findings in two families. Partial restoration of cardiovascular perform by embryonic neural stem cell grafts after full spinal cord transection. Upper mind stem compression and foraminal impaction with intracranial space-occupying lesions and mind swelling. Filaments in siderotic nodules of spleen in circumstances of splenomegaly of unknown origin. Radial glial cell transformation to astrocytes is bidirectional: regulation by a diffusible think about embryonic forebrain. Feasibility of cell therapy in multiple sclerosis: a scientific review of 83 studies. Sustained astrocytic clusterin expression improves transforming after mind ischemia. Perisulcal infarcts: lesions brought on by hypotension throughout elevated intracranial pressure. The pathology of encephalic arteriovenous malformations handled by prior embolotherapy. Glial fibrillary acidic protein mutations in infantile, juvenile, and adult forms of Alexander illness. Role of microglia in inflammation-mediated neurodegenerative illnesses: mechanisms and techniques for therapeutic intervention. Increased technology of neuronal progenitors after ischemic harm in the aged adult human forebrain. The position of intermediate progenitor cells within the evolutionary enlargement of the cerebral cortex. Oligodendrocytes and progenitors turn out to be progressively depleted inside chronically demyelinated lesions Am J Pathol 2004;164:1673�82. Moderate and extreme traumatic mind damage: epidemiologic, imaging and neuropathologic perpectives. Postnatal cerebral cortical multipotent progenitors: regulatory mechanisms and potential position within the improvement of novel neural regenerative strategies. Axonal plasticity and functional recovery after spinal wire damage in mice poor in both glial fibrillary acidic protein and vimentin genes. Vascular lesions of the mind stem and occipital lobe occurring in affiliation with mind tumours. Radial glia and somal translocation of radial neurons within the growing cerebral cortex. Neurovascular unit dysfunction with blood�brain barrier hyperpermeability contributes to major depressive dysfunction: a evaluate of clinical and experimental proof. In vitro proliferation of axotomized rat facial nucleus-derived activated microglia in an autocrine trend. Neural exercise triggers neuronal oxidative metabolism followed by astrocytic glycolysis.
Buy brahmi mastercard
A rich submucosal venous plexus, deep to the nasal mucosa, provides venous drainage of the nose via the sphenopalatine, facial, and ophthalmic veins. Venous blood from the external nose drains mostly into the facial vein by way of the angular and lateral nasal veins. However, recall that it lies throughout the "danger area" of the face because of communications with the cavernous (dural venous) sinus (see the scientific box "Thrombophlebitis of Facial Vein"). Regarding the nerve provide of the nostril, the nasal mucosa can be divided into postero-inferior and anterosuperior portions by an indirect line passing roughly via the anterior nasal backbone and the spheno-ethmoidal recess. The nerve provide of the postero-inferior portion of the nasal mucosa is chiefly from the maxillary nerve, by means of the nasopalatine nerve to the nasal septum, and posterior superior lateral nasal and inferior lateral nasal branches of the larger palatine nerve to the lateral wall. The olfactory nerves, involved with odor, arise from cells within the olfactory epithelium within the superior part of the lateral and septal walls of the nasal cavity. The central processes of those cells (forming the olfactory nerve) pass through the cribriform plate and end within the olfactory bulb, the rostral expansion of the olfactory tract. An open-book view of the lateral and medial (septal) walls of the best facet of the nasal cavity is proven. Paranasal Sinuses the paranasal sinuses are air-filled extensions of the respiratory a half of the nasal cavity into the following cranial bones: frontal, ethmoid, sphenoid, and maxilla. The sinuses continue to invade the encircling bone, and marked extensions are common within the crania of older individuals. The right and left sinuses every drain by way of a frontonasal duct into the ethmoidal infundibulum, which opens into the semilunar hiatus of the middle nasal meatus. The paranasal sinuses of the best side have been opened from a nasal method and 2174 color coded. An anterior ethmoidal cell (pink) is invading the diplo� of the frontal bone to turn out to be a frontal sinus. Radiograph of cranium demonstrating air densities (dark areas) associated with paranasal sinuses, nasal cavity, oral cavity, and pharynx. The frontal sinuses range in dimension from roughly 5 mm to massive areas extending laterally into the higher wings of the sphenoid. Often, a frontal sinus has two elements: a vertical half in the squamous part of the frontal bone, and a horizontal part within the orbital part of the frontal bone. When the supra-orbital part is large, its roof forms the floor of the anterior cranial fossa and its flooring forms the roof of the orbit. The anterior ethmoidal cells drain immediately or not directly into the middle nasal meatus by way of the ethmoidal infundibulum. The center ethmoidal cells open directly into the middle meatus and are typically referred to as "bullar cells" as a outcome of they kind the ethmoidal bulla, a swelling on the superior border of the semilunar hiatus. The ethmoid bone occupies a central place, with its horizontal component forming the central part of the anterior cranial fossa 2176 superiorly, and the roof of the nasal cavity inferiorly. The ethmoidal cells give attachment to the superior and middle concha and type a part of the medial wall of the orbit. The maxillary sinus varieties the inferior part of the lateral wall of the nose and shares a standard wall with the orbit. The center concha shelters the semilunar hiatus into which the maxillary ostium opens (arrow). Because of this extensive pneumatization (formation of air cells), the physique of the sphenoid is fragile. Only skinny plates of bone separate the sinuses from a number of essential constructions: the optic nerves and optic chiasm, the pituitary gland, the inner carotid arteries, and the cavernous sinuses. The sphenoidal sinuses are derived from a posterior ethmoidal cell that begins to invade the sphenoid at approximately 2 years of age. In some folks, several posterior ethmoidal cells invade the sphenoid, giving rise to multiple sphenoidal sinuses that open separately into the sphenoethmoidal recess. They occupy the bodies of the maxillae and talk with the middle nasal meatus.
Real Experiences: Customer Reviews on Brahmi
Hauke, 58 years: If essential, traction of the ureters is applied gently and only towards the blood provide to avoid disruption of the small branches. The gastrocnemius and soleus share a common tendon, the calcaneal tendon, which attaches to the calcaneus. Thus, most muscle tissue are composed of multiple myotome, and most often, multiple spinal wire segments are concerned in producing the motion of the decrease limb. The cricothyroid is supplied by the exterior laryngeal nerve, one of the two terminal branches of the superior laryngeal nerve.
Folleck, 38 years: During passage of the fetus via the start canal, the halves of the frontal bone turn into flat, the occipital bone is drawn out, and one parietal bone barely overrides the opposite. When current, this small artery ascends on the anterior floor of the trachea, supplying small branches to it. They are often found incidentally at post-mortem as small areas of reddish blush, most incessantly in the foundation pontis and more hardly ever in different parts of the mind and spinal cord. The rectum lies posteriorly in opposition to the inferior three sacral vertebrae and the coccyx, anococcygeal ligament, median sacral vessels, and inferior ends of the sympathetic trunks and sacral plexuses.
Denpok, 33 years: Relapsing and remitting a quantity of sclerosis: pathology of the newly forming lesion. These principally sensory nerves also carry parasympathetic secretomotor fibers to serous glands within the tongue. The trapezius is a large, flat triangular muscle that covers the posterolateral facet of the neck and thorax. Branchial Sinuses and Cysts When the embryonic cervical sinus fails to disappear, it might retain its reference to the lateral floor of the neck by a branchial sinus, a slim canal.
Deckard, 35 years: The nerves derive from the S2�S4 spinal cord segments and spinal ganglia, passing through the pelvic splanchnic and pudendal nerves, respectively. The extensors of the hip and flexors of the knee contract eccentrically on the finish of swing section (terminal swing;. The inferior extensor retinaculum, a Y-shaped band of deep fascia, attaches laterally to the anterosuperior surface of the calcaneus. It is helpful to notice that although the blood supply to the belly section of the ureter approaches from a medial direction, that of the pelvic phase approaches from a lateral direction.
Kent, 48 years: The transverse processes of all cervical vertebrae (typical or atypical) include foramina transversaria for the vertebral vessels (the vertebral veins and, aside from vertebra C7, the vertebral arteries). The frontal suture divides the frontal bones of the fetal skull (see the clinical field "Development of Cranium"). To visualize the scale of this opening, notice that that is barely bigger than essential to permit the passage of a 2- � 4inch piece of lumber. The inferior wall (orbital floor) is fashioned primarily by the maxilla and partly by the zygomatic and palatine bones.
Bradley, 55 years: Infratemporal Fossa the infratemporal fossa is an irregularly shaped house deep and inferior to the zygomatic arch, deep to the ramus of the mandible, and posterior to the maxilla. Each inside carotid artery enters the cranial cavity by way of the carotid canal in the petrous a half of the temporal bone. At 2 months, the undifferentiated gonads (primordial ovaries) are positioned on the dorsal belly wall. In these circumstances, the morula (early embryo) could not be in a position to cross alongside the tube to the uterus, although sperms have obviously accomplished so.
9 of 10 - Review by O. Nefarius
Votes: 331 votes
Total customer reviews: 331


